We have a lot to learn about the distal radio-ulnar joint (DRUJ) which is part of the forearm rotation movement. If you keep the elbow at a right-angle and rotate your hand from palm up to palm down, this is known as supination and pronation. What happens is that the radius, the bone on the thumb side of the forearm rotates around the ulna, which is on the little finger side. For this to happen the radius rotates at the elbow (the radio-capitellar articulation) and at the wrist (the DRUJ) but also there is a membrane (the interosseous membrane) that twists as well. All three structures must be working properly for forearm rotation to occur. There are many conditions which can affect this movement and we hope to address these in detail.
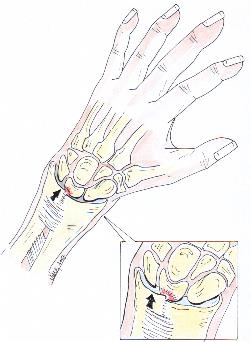
Normally the ulnar head does not have any contact with the carpal bones in the wrist and is separated from them by an important trampoline-like structure formed of cartilage. This is very similar to the cartilage in the knee known as the ‘meniscus’ and it is referred to in the wrist as the triangular fibrocartilage complex (TFCC).
The TFCC can undergo degeneration through progressive wear and then tear. If this happens the ulnar head can then rub against some of the carpal bones, in particular, the lunate bone, and cause pain and arthritis. This is dependent on the relative length of the ulna to the radius. Some people have a naturally too-long ulna or due to a previous fracture to the radius (which can become shorter) it becomes relatively too long causing damage to the TFCC. A tear occurs which may eventually affect the joint surfaces as well. All kinds of people can suffer problems of the DRUJ, young and old; active and inactive but fortunately not all of them need surgery.
Diagnosing TFCC tears can be difficult and, if found, not all tears can or need to be treated. If we think you may be suffering from such a tear we perform routine x-rays of the wrist and in some instances an MRI. Occasionally we may take a look inside your wrist by performing an arthroscopy. Some tears only require trimming but some will require formal repair. If it is possible to repair the tear, with prior agreement we will do it then and there. If it cannot be repaired arthroscopically then open surgery is an option either at the same time as the arthroscopy or at a later stage. This would mean you would have to wear a long-arm cast for at least 4 weeks following surgery and then a removable forearm splint for another 4 weeks.
As mentioned before some people have a naturally too-long ulna or acquire this due to a previous injury to the forearm. This can result in the ulnar head perforating the overlying cartilage and cause “impaction” into the lunate bone. It may be related to activities that involve a lot of movement of the wrist in a 'cocking' up and down motion in the plane of the thumb.
If we feel you may be suffering from such a problem we will conduct specialized x-rays in different positions and probably a MRI scan to determine the presence or extent of the damage. Distinguishing between ulnar impaction syndrome and other potential causes can be difficult and sometimes arthroscopy will be required as well. Treatment usually consists of a modification of activity so that you avoid stressing this area too much, anti-inflammatory drugs, splints and sometimes a corticosteroid injection. Surgery is indicated when everything else fails. Surgery involves either shortening the ulna head arthroscopically, by removing a “wafer” of bone or openly cutting out a 2-3 millimetre segment at the mid-shaft level of the ulna. This requires the bone to be fixed with a plate and screws.
The recovery from the arthroscopic procedure is much shorter but its success depends on a number of factors. There has to be a central tear of the TFCC to allow the surgeon to see the ulna head from inside the wrist joint (specifically the radio-carpal joint) and it is critical that there is no instability of the DRUJ itself. Thus it may not be technically possible to perform the ulna shortening arthroscopically and the open procedure is required. We will advise you about these issues prior ro deciding on surgery. If open shortening is performed a half cast (back-slab) is worn for two weeks followed by a protective splint for at least a further four.